SmarterDx is now proudly part of Smarter Technologies
LEARN MORE
Every year, denial rates climb, leaving hospitals fighting for lost revenue. Enter SmarterDenials™, the clinical AI that gives hospitals a faster, more efficient way to overturn denied claims and recover lost revenue by automatically generating evidence-backed clinical appeal letters.
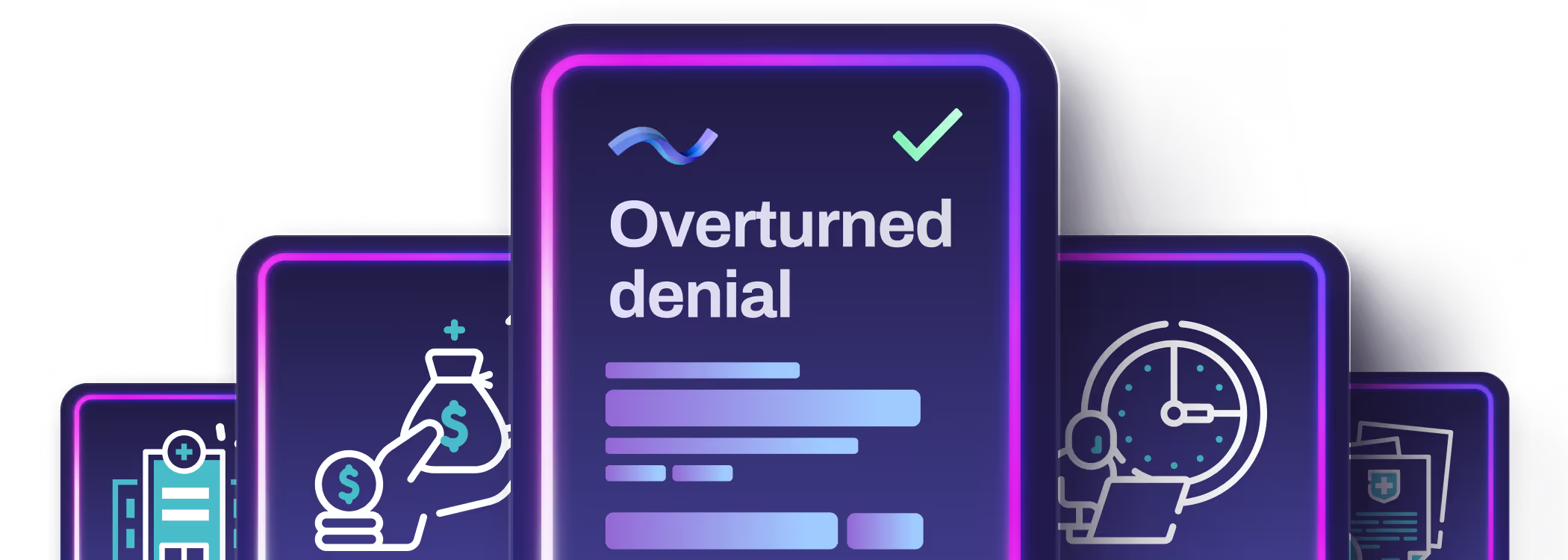
Quickly identifies discrepancies between the denial and the documented care.
Automatically generates letters backed by the clinical evidence and coding references needed to win, even for the most complex cases.
Our generative AI creates appeal letters in just minutes.
SmarterDenials drastically reduces time and paperwork, but your team has full control — reviewing, refining, and sending the final letter.

Crafting appeals the traditional way means hours spent sifting through patient charts, clinical notes, and coding rules — just to make your case.
SmarterDenials flips the script. In minutes, it creates comprehensive, compelling appeals for even the most complex cases, helping your hospital get paid more and paid faster. As payers tighten their criteria, you need a tool that fights back with speed, precision, and results.
Empower your team to win more appeals, slash administrative headaches, and recover more revenue, all while freeing your staff to focus on what really matters: patient care.
Even if it’s a fax or pixelated scan, SmarterDenials extracts key data to build effective appeal arguments.

Analyzes the denial and the complete patient record, including provider notes, labs, meds, orders, vitals, and more.
Identifies key clinical evidence to help your team quickly understand how the patient record supports the claim(s).

Creates a comprehensive clinical appeal letter in minutes that the team can view, edit in the SmarterDx web app, and copy or download to send.

Whether it's a DRG downgrade or a level of service denial, SmarterDenials provides the necessary clinical evidence and coding references to support the appeal — so your team can focus on patients, not paperwork.
Ready to learn more? Get in touch with us today and we’ll set you on the path to revenue integrity.